NAVIGATING THE RIP OF COVID-19 ISOLATION
/in Uncategorized /by Vincent King

A beep signalled an SMS with the awaited results of my recent PCR test. I was struck immediately with shock, surprise and disbelief. It was positive. Throughout my life, during challenging times, I have always defaulted to pragmatism rather than panic. So, on receiving this news, I took a deep breath, sat down with my partner and worked out an action plan.
Like being in a rip in the ocean, the more we fight and resist the harder we make it. Being in iso can be the same. We can’t control our circumstances, but we can control how we respond to them.
As a health care practitioner, I was an early adopter, jumping at the chance to be vaccinated and receive the booster when it was available to me. So, despite testing positive to Covid-19, I knew my chances were good.
While I navigate iso, over the coming days I’ll share with you some ways to best prepare for the day you receive that SMS notice when your Covid-19 test returns positive and what to expect.
PREPARE
The government recommends treating mild Covid-19 symptoms like you would a seasonal flu with paracetamol or ibuprofen. A little while ago, my partner and I created a COVID-19 supplies box with all the medicines and paraphernalia we would need for this day. Please speak to your GP to see if these are suitable to your specific circumstances:
: Rapid Antigen Tests for household contacts
: Thermometer
: Pulse oximeter
: Ibuprofen
: Paracetamol
: Throat lozenges
: Betadine sore throat gargle
: Hydralyte
: N95 masks
Freezing bulk cooked meals is also a great idea and an enormous help during iso. Bolognese, lasagne and frozen New Zealand whiting fillets whiting fillets are my favourite options.
If you are asymptomatic or feel well enough, there are ways to keep active within your home. I’m using resistance tubes to help stretch and stay strong. You can purchase these from The WOD Life https://www.thewodlife.com.au/collections/the-wod-life/products/resistance-tubes. Foam rollers are also a great way to iron out stiff and tight muscles.
COMMUNICATIONS
The first comms you will receive from NSW Health will be an SMS alerting that you returned a POSITIVE result for COVID-19. It will ask you to complete the form through a link in the SMS which will triage your health risk factors.
You will also be asked to self-isolate for 7 days starting from the date you had the RAT or PCR test. This isolation requirement will include anyone else in your household or other close contacts. If your symptoms, including sore throat, runny nose, cough or shortness of breath, continue after the 7 days you will need to remain in self-isolation until all those symptoms clear.
If you develop severe symptoms such as shortness of breath or chest pain, call triple zero (000) immediately.
LOGISTICS
Don’t hurt the ones you love. Become your own contact tracer. Alert those who you had more than 4 hours recent contact with that you have tested positive, as they are now identified as close contacts. They will be required to also isolate for 7 days and get a RAT or PCR test.
Lean on your friends. Reach out to someone to be your logistics person on the “outside” for groceries or supplies. If they like you a lot, they may even bless you with delivering home cooked meals.
I know it seems illogical and counter intuitive but despite living in the same house, your household contacts or intimate partner may not have contracted COVID-19. Try to keep as separate from them as much as possible by isolating in a separate room and everyone should wear a N95 mask. Despite testing positive, my partner, who I live with, has tested negative on 2 x RATs and 2 x PCR tests. COVID-19 works in mysterious ways.
MENTAL WELLBEING
During iso, feelings of being alone or in a silo can come up. Form your own community by reaching out to friends and family, particularly to others isolating at the same time. A shared experience can lighten the burden. We have formed a What’s App group with others who are isolating as well.
Make a Telehealth appointment with your GP to get assessed for a mental health care plan to access psychology services under Medicare.
RECOMMENDATIONS
Rest. Drink water. Eat and rest some more.
Your body’s immune system, with the help of the vaccine, will do all the hard lifting fighting the virus. Help them by being kind to yourself.
If you develop severe symptoms such as shortness of breath or chest pain, call triple zero (000) immediately.
In my iso I am fortunate to currently be asymptomatic. If you find yourself in this place here are some recommendations that are keeping me sane:
: Yoga with Adriene. Adriene and her lovely Blue Healer dog Benji offer free YouTube yoga videos. She leads a calm, non-competitive guide to yoga.
: Insight timer meditation phone app
: Resistance tube exercises. I’ll be sharing some home training videos on this very soon.
FINAL NOTES
The thing my partner and I are looking forward to once we exit iso this weekend is immersing ourselves in the saltwater of Maroubra Beach.
Iso is teaching me how to be a good support person should one of my friends or loved ones go into isolation. Nothing will stop me from delivering gifts of fruit, veggies and home cooked meals made with love, understanding and blessings for a full recovery.
Welcome Rebecca Bau
/in Uncategorized, Acupuncture, Japanese Acupuncture, Chinese Herbal Medicine lohan, qigong, unable, health, bau, medicine, welcome, chinese, everyday, acupuncture, rebecca, lohan qigong, rebecca bau, eastern /by admin_wmcWelcome back to Rebecca Bau
We are pleased to welcome back Rebecca Bau to our Wholistic Medical Centre team!

Rebecca is an acupuncturist, Chinese herbalist and Lohan Qigong practitioner who integrates eastern life philosophies and eastern medicine practices for everyday health and wellbeing.
She brings clinical skills in Acupuncture, Japanese Acupuncture, Moxibustion, Shonishin, Chinese herbal medicine and Lohan Qigong which she has practiced for over 15 years.
Rebecca has been a part of many amazing stories, primarily in women’s health assisting with fertility, pregnancy and labour. However, in practice she treats people of all ages and conditions… Her youngest patient was a 9mth old baby who had digestive upsets unable to gain weight, and the eldest a 97yr old with shoulder pain unable to go for their everyday swim.
To find out more about Rebecca’s experience and her treatment consultations, click here.
Anxiety during pregnancy
/in Uncategorized acupuncture, see, pregnancy, helps, perinatal anxiety, point, prevalence, perinatal, anxiety, women, therapy /by Kyla MayerPregnant & overwhelmed?
You are not alone, with an estimated 1 in 5 women reporting anxiety symptoms throughout their pregnancy & anxiety prevalence peaking during third trimester, anxiety is more common than we think. Expecting mother have also had to face many changes and restrictions to their care delivered during Covid-19 and these unique times have added to the prevalence of perinatal anxiety.
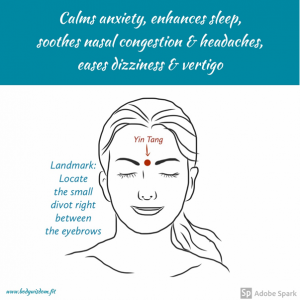
Now, one well known therapy that can assist with anxiety and slow down the parasympathetic nervous system (fight or flight response) and silence those bust thoughts is acupuncture. Acupuncture that is considered safe to use in pregnancy, although there can be risks involved, such as localised redness at the needle insertion point. Most women find acupuncture gentle, although some are more sensitive than others, as the needles used are very fine. But acupuncture and can provide support for perinatal anxiety and permission to stop and rest when life can be overwhelming…
If you want to test & see if this is the right therapy for you try massaging this point directly between your eyebrows for 3 minutes and see if this acupuncture point helps.
Hope this helps! Remember, you got this, mamma.
FERTILITY MASSAGE – WHAT IS IT ALL ABOUT?
/in Remedial massage, Shiatsu and Chinese massage (Tui Na), Uncategorized organs, ideal time, improves organ function, ideal time for fertility, fertility massage, time for fertility, menses to ovulation, ideal time for fertility massage, trying to conceive, time for fertility massage, physical body, fertility massage therapist, improves organ, massage therapist, organ function, pelvic organs, massage, fertility massage therapy, conceive, massage therapy /by Kyla MayerIf you have been trying to conceive you will know how much it takes its toll on you, both emotionally and physically.
You may have been trying naturally to conceive or gone through the channels of IVF. Either way, the longer this cycle of trying goes on, the more your mind can panic emotionally sending you into overwhelm and distress.
When trying to conceive, the physical body and hormones are tested, examined, poked and prodded, your BMI, weight and age is recorded and your physical body is relied on to get you pregnant. However very little is paid to the emotional side of your journey and this can be the biggest key to falling pregnant. The pressure and expectations to conceive can be cripplingly stressful and this is where fertility massage and be of great assistance.
Fertility Massage Therapy
Fertility Massage Therapy is a deep, yet gentle and non-invasive therapy that works by bringing the organs within the abdominal area back into alignment, releasing pressure and strengthening the surrounding muscles and ligaments.

Some of the benefits of fertility massage
- Fertility Massage Therapy aims to re-position your internal abdominal organs, including the uterus, as the positioning of your uterus helps optimise your chances for fertilisation and implantation.
- Improves organ function by releasing physical & emotional congestion from the abdomen.
- Improves circulatory, lymphatic & nervous systems by encouraging more blood flow to reproductive & pelvic organs by resolving any congestion & misalignment to these organs.
- Helps to tone & strengthen the uterus & surrounding ligaments to optimise fertilisation & implantation.
- Breaks down scar tissue or adhesions surrounding reproductive, digestive & pelvic organs which improves organ function & health.
- Helps to subdue parasympathetic nervous system & induce rest & relaxation….which is always welcome.
WHEN TO HAVE FERTILITY MASSAGE
If you are trying to concieve naturally…
….the ideal time to have fertility massage is the end of menses to ovulation. This is commonly from day 7 to day 14 of your cycle.
If you are undergoing fertility assistance…
….with IUI the ideal time for fertility massage is from menses to ovulation & insemination.
…. with IVF then the ideal time for fertility massage is from suppression of your cycle to embryo transfer is recommended, as long as no tenderness is felt.
Our Fertility Massage Therapist
Kyla Mayer is our skilled and experienced fertility massage therapist. Kyla has a special interest in pregnancy & remedial massage, lactation support, pregnancy, women’s health, fertility, acupuncture and traditional Chinese medicine and you can read more about her here.
To book an appointment with her you can call (02) 9211 3811 or book online here.
We are pleased to introduce you to Simone Jeffries who joined our team at the Wholistic Medical Centre in March 2020.
/in Uncategorized conditions, loves to inspire, simone, loves, inspire, health, working, medicine, naturopath, women, digestive, children /by admin_wmc
Simone is a naturopath who has a special interest in digestive disorders and women’s health. Simone combines functional testing, herbal medicine and nutritional recommendations to support improvements in a wide range of health conditions. She is also a certified wellness coach and loves to inspire her clients to be the healthiest version of themselves.
Many women in their 40s and 50s chose Simone as their naturopath because she has focussed on building proficiency in supporting women with menopause and digestive conditions.
As a mother of 3 grown up children, Simone also enjoys working with children and teenagers. She has experience working with common childhood illnesses, ADHD and skin conditions such as acne and eczema.
Simone also loves to educate teenage girls about their menstrual cycle and teach them how to manage PMS, PCOS, anxiety and digestive problems using nutrition and stress management techniques.
As a lifelong herb gardener and foodie, Simone brings her passion for herbs and vegetables into the clinic and loves to inspire people to maintain a healthy balance by understanding how to use food as medicine.
To read more about Simone and the conditions she works with, click here.
After the Birth. What now? Tips to help you through the Golden Month.
/in Uncategorized new mother, lower the heat, parmigiano-reggiano cheese, mothers, salt and pepper, heat, soup, recovery, postpartum period, chicken soup, baby, 1 garlic, mother, 1 handful, olive oil, continental parsley, stock, chicken, birth of their baby, new mothers /by Kyla MayerThe Golden Month after your baby is born
Many women feel exhausted & overwhelmed after the birth of their baby and their recovery is overshadowed by the desire to ‘bounce back’. In modern society women are praised and admired for how quickly they are up and at ‘em and looking great post the birth of their baby. This modern day phenomenon is contrary to many traditional cultures where it is common place for the new mother to do nothing more than rest, feed and bond with her baby. In traditional Chinese medicine this is known as the Golden Month and new mothers are given special care, food and support until they feel recovered. This month is seen as providing valuable health benefits and allowing a new mother to adjust to her new role regardless if this is her first or third child. As every child, pregnancy & childbirth will be different, the needs of every new mother will differ. This is a time to recuperate and it is important to promote a mothers physical & emotional wellbeing. This is an opportunity to address any health needs that the mother may experience in the recovery from childbirth and start the journey to motherhood supported and confident.
What assists a new mother in her recovery in the postpartum period can be simplified in four basic tips:
Rest
Every new mother is told to sleep when your baby sleeps. This is essential for recovery as newborn babies will breastfeed at all different hours and sleep when you don’t think they should. Lie down for a day sleep with your baby as this will not only encourage bonding but will provide you with some valuable rest.
Nutritious food
New mothers need good nutrition. A combination of carbohydrates, protein & good fats to encourage a good milk supply & provide the needed nutritional needs that are amplified while breastfeeding and recovering from childbirth.
Hydration
New mothers need at least 10 -12 glasses of water each day to satisfy their fluid requirements in the postpartum period. This is to promote lactation as well as assist the heart and kidneys to flush all that extra fluid and interstitial fluid that accumulates in the final weeks of the pregnancy.
Reach out to your tribe & accept help
It is so important to create a supportive circle of people. They can assist in providing nutritious meals during this time that can be easily frozen and eaten anytime, especially when cooking cannot be managed. This is essential for your physical and emotional recovery. Reach out to your mothers group & local breastfeeding support groups in your local early childhood centres as this can be a great source of support & connection with other local mothers. Remember you are not alone and don’t hesitate to ask for and access the help you need.
RECIPE FOR NONNA’S CHICKEN SOUP
This brings such memories from watching my grandmother skim the pot of her chicken broth & one that will bring you nourishment, warmth, health & happiness.
BRODO DI POLLO – ITALIAN CHICKEN SOUP
For stock and soup:
- 1 whole chicken
For stock:
- 2 carrots, peeled and halved
- 3 celery stalks, rinsed and trimmed with leaves removed, then quartered
- 1 fennel bulb, stalks removed, then quartered
- 1 garlic bulb, halved widthways
- Rind from a wedge of Parmigiano-Reggiano cheese *
- 2 bay leaves, fresh or dried
- 1 handful continental parsley and stalks
- 1 teaspoon peppercorns
For soup:
- 2 tablespoons extra virgin olive oil
- 1 medium brown onion, diced
- 1 garlic clove, minced
- 2 medium carrots, diced
- 2 celery ribs, diced
- 1/3 cup dried risoni pasta
- Salt and Pepper to taste (to serve)
- 1 handful fresh continental parsley (to serve)
- 1/4 cup grated Parmigiano-Reggiano cheese (to serve)
STOCK
Place chicken and vegetables in a large stockpot over medium heat. Top with cold water till just covered (don’t add too much water or the stock will be weak in flavour). Add remaining stock ingredients and let it slowly come to the boil. Lower the heat to a gentle simmer and cook for 1 hour, partially covered. While simmering, skim the surface of the liquid once or twice to remove any impurities that rise to the surface. Top with more water if required to keep the chicken just submerged.
Remove the chicken to a cutting board and allow to cool for a few minutes. When it has cooled, discard the skin and bones and shred the meat with a fork. Set aside in a covered container.
Strain the stock through a fine sieve into a large bowl to remove the vegetables and aromatics and set aside. Then, wash and dry your stockpot.
SOUP
Heat olive oil in the stock pot over medium high heat, then add the onion, garlic, carrot and celery and sauté till the onion is translucent but before the mirepoix browns. Lower the heat to medium-low and add the stock to the pot with the shredded chicken and the risoni. Simmer until the risoni is cooked (about 11 minutes, but follow the timing on the pasta packet).
Remove from heat, season to taste with salt and pepper and stir through the cheese and finely chopped parsley then divide between four bowls.
*I keep the rind from finished Parmigiano-Reggiano cheese segments in the freezer for whenever I need to add flavour to simmering soups.
Where are we up to with medicinal cannabis?
/in Uncategorized, General Practice, Integrative Medicine medical centre, authorised, medical, prescriber, australia, kotsirilos, gp, gps, medicinal cannabis, cannabis, medicine, primary dysmenorrhoea, period pain, medicinal, pain, clinical, wholistic medical centre, pathways, wholistic medical, scheme /by admin_wmc
Is it legal? 
Medical practitioners in Australia can legally prescribe medicinal cannabis through regulated pathways such as the Special Access Scheme Category B and the Authorised Prescriber Scheme. These pathways are typically used by doctors for unapproved medicines.
Dr Vicki Kotsirilos, Victorian GP and Integrative Medicine Practitioner, became Australia’s first authorised GP prescriber of medicinal cannabis in May 2018. She said recently that GPs currently have ‘a large demand’ for knowledge about the use of medicinal cannabis. Dr Kotsirilos says there is a lack of knowledge about the clinical usage of medicinal cannabis which stems from a lack of formal education and upskilling available to GPs.
‘We need regular top-ups of education because the science actually changes every day and there’s new studies that come out all the time,’ she said. ‘Because it is a plant medicine, it’s not part of our curriculum, so all the learning is self-taught.’
What is it currently prescribed for?
The main medical conditions for which medicinal cannabis is prescribed in Australia to date are:
- chronic non-cancer pain
- epilepsy
- multiple sclerosis
- palliative care including cancer pain management
- cancer-related nausea and vomiting.
Is it available at Wholistic Medical Centre?
We are very fortunate that Dr Nick Bassal, who had already begun upskilling in the use of medicinal cannabis, has been invited to participate in a conference in Montreal, Canada, taking place as this newsletter goes to ‘print’. So, watch this space if you believe that you have a need for medicinal cannabis.
Medical cannabis for period pain? Would you like to have your say?
‘Development of a clinical trial on medicinal cannabis for primary dysmenorrhoea: Co-Design.’
Researchers from NICM Health Research Institute would like to invite women who suffer from ‘primary dysmenorrhoea’, that is period pain not due to endometriosis or adenomyosis, to participate in an on-line focus group to have your say in how clinical trials should be designed to be relevant and well-structured. Read the participant information at https://nicm.edu.au/__data/assets/pdf_file/0007/1615795/Participant_Information_Sheet_MC_and_Period_pain_V2.pdf
Or ask our wonderful Reception Team at the Wholistic Medical Centre for more details.
When your baby is breech in the final weeks of pregnancy …. Acupuncture, TCM and massage may help.
/in Uncategorized pubic symphysitis, persistent breech, initial treatment, right hip, postural techniques, head first position, application of moxabustion, traditional chinese medicine, confident to continue, chinese medicine, natural birth, traditional chinese, breech baby, baby, turning baby, amy, external cephalic, persistent breech baby, cephalic version, external cephalic version /by Kyla Mayer
Turn baby, turn….
Most women hope for a natural birth, but what happens when a persistent breech baby puts a spanner in the works?
As your pregnancy progresses, your baby naturally turns into the head-first position. However, a small number of babies will not turn and remain in a persistent breech position, or bottom first, in the final weeks of pregnancy. There are a variety of reasons for this ranging from placental location, fibroids or uncommon-shaped uterus, laxed uterine muscle tone from multiple pregnancies or lots of fluid around baby in utero.
This can be a source of great stress and anguish for a woman in those last weeks of pregnancy as discussions around turning baby (External Cephalic Version) and alternative delivery plans may arise.
Amy’s story
Amy* was 35 weeks pregnant with her third baby when she came to see me with a persistent breech baby on board. She had been discussing her choices and delivery plan with her Obstetrician and was wanting to wait and see if her baby would turn head first within the following weeks. A normal birth was what she really wanted and an External Cephalic Version did not appeal to her.
Her Obstetrician agreed to give Amy three weeks to see if her baby would turn. This is when she came to see me. Her Obstetrician was informed that Amy was seeking my assistance and was not resistant to her trying massage or acupuncture.
Baby’s head needed room
I approached the consultation as I always do with a thorough medical history and background of Amy’s condition. I had discovered that Amy had suffered from pubic symphysitis with each of her three pregnancies. This prompted me to thoroughly assess Amy’s hips and pelvis position and function as these may lead to a narrowing of the pelvic outlet thus reducing the baby’s ability to turn headfirst. They can also be the source of severe pain.
I commenced my assessment by comparing both hips for symmetry, movement and position and observed that Amy’s right hip was sitting slightly higher and turned toward the front when compared to the left hip. When I observed Amy walking, there was a tendency for her to raise her right hip higher than her left when taking a step forward. This confirmed my suspicions that the hips had been drawn out of alignment during pregnancy while under the affect of pregnancy hormones.
This was placing strain on Amy’s pelvis and making her gluteal muscle groups work hard to support her when she was walking.
I began the treatment by massaging her lower back and hips, focusing on the gluteal muscles to improve blood circulation and movement of smooth muscle tissue. This was aimed at reducing discomfort and allowing the hips to move more freely as well as targeting hip alignment.
Very motivated to help the baby to turn
After discussion with Amy and understanding her commitment to turning her baby to the head first position, I decided to introduce acupuncture and moxibustion into the treatment to amplify the focus on turning baby and realigning the right hip.
Acupuncture was applied also to reduce the pubic symphysitis pain. I have found this to be very effective over my years in practice. Acupuncture is complementary medical practice that involves stimulating certain points on the body, most often with a needle penetrating the skin to alleviate pain or to help to treat various health conditions.
The final layer to the initial treatment was moxabustion and this was applied while Amy was comfortable lying on her side and the acupuncture needles were in place. Moxabustion is used in Traditional Chinese Medicine to stimulate specific therapeutic effects and is the practice of burning a herb called Artemesia vulgarisacross certain acupuncture points. The application of moxabustion increases blood flow creating an environment of movement and activity in the growing baby promoting optimal positioning in utero. The key point to stimulate to assist with turning the baby is BL67 located on the outer corner of the fifth toe.
The recommended application of moxabustion is 20 mins daily for 10 days in succession. I performed the initial application so that Amy was confident to continue using it at home independently and tolerated the treatment. As with burning any substance it was important that Amy knew exactly where to place it and how much heat the moxabustion should generate on the skin.
After this initial treatment Amy felt confident to continue using the moxabustion treatment and tolerated this therapy well. Her baby did move around a lot during the treatment and I was hopeful that baby would settle head first over the next 9 days. At the conclusion of the appointment I also gave Amy instructions on postural techniques that she could adopt at home to encourage baby to turn into the head first position. I included some instructional videos for her to follow.
Another postural technique that I recommended to Amy was the cat stretches which help with pelvic pain and strain by again tilting baby off the lower back and pelvis to relieve pain. Once again I gave her some resources to support her doing the technique correctly. I explained that she should attempt these techniques daily for at 10 mins at a time to achieve optimal results.
Amy returned to see me after the 10 days of moxabustion application and postural techniques. She was very happy to report that the baby had turned head first. This was a testimony to her commitment and compliance with the treatment. Her Obstetrician was pleased.
Amy proceeded to a natural birth of her baby – head first!
* Name has been changed
By Kyla Mayer – Pregnancy and Remedial Massage, Lactation Consultant, Acupuncture and Traditional Chinese Medicine – Red Tent inside Wholistic Medical Centre
Healthy Green Soup recipe
/in Uncategorized cover vegetables, salt, stock, pepper, spinach, taste, parsley, vegetables, salt pepper to taste, bunch, pepper to taste, garnish, 1 bunch, garlic, olive oil, olive, salt pepper, oil, nutritional yeast, chickpeas /by admin_wmc
Ingredients
1 Fennel bulb
1 Head of broccoli
1 Zucchini
1 Bunch of English Spinach
1 Bunch of Parsley – keep a little parsley to garnish.
4 Cloves of garlic
1 Tbspn olive oil
1 Tin of Chickpeas 440g
2-3 cups of stock (Vege or chicken – you choose)
Salt & pepper to taste
Optional – Nutritional Yeast or Parmesan
Method
Chop garlic and fry gently in olive oil, add roughly chopped vegetables and stock. Ideally stock should just cover vegetables – I put everything in except the spinach then add stock to cover vegetables. Throw the spinach in on top as it reduces quite dramatically in size.
Simmer until tender. Add chickpeas, salt & pepper to taste. Blend.
A stick blender is ideal to create a fabulous green soup.
I like to add nutritional yeast just before serving or you may like to add parmesan.
Garnish with parsley.
By Lucy Bella – Wholistic Medical Centre Office Manager
How my ebike, affectionately known as “The Beast”, changed my world
/in Uncategorized shop, lights, vest, wholistic medical, medical, wholistic, ebike, ride, pootle, bicycle, power /by admin_wmc
On a trip to Canberra I hired an ebike to ”pootle” around (a term I had not come across before but my friend assured me was the correct description for ambling around on a bicycle with no express purpose or intention).
It was love at first sight – the Kalkhoff was a step-through with a generous sprung seat and ample carry basket at the rear, three power selections and a it was lovely charcoal gray. The top power setting meant that no hill was too steep for me to tackle.
We proceeded to ”pootle” around the city and suburbs and by the end of my weekend I was googling where I could buy one in Sydney.
Shout out to the Dutch Bicycle shop – Omafiets at 17 George St, Redfern.
My old Giant was retired and instead of just doing a ride on weekends I now began to commute to work. Luckily part of my journey to Wholistic Medical Centre goes through Centennial Park. This has become the highlight of my day – twice a day. On the morning ride I usually check in on the flock of geese to see what shenanigans they are up to and to listen to their communal honkings. On the return I get to whizz through the ghost gums with my lights casting eerie shadows.
I have found that my headspace is markedly improved by the big sky experience and the gentle exercise that commuting by ebike has offered me.
Then of course we come to the accessories – initially I had the high vis vest that all the construction workers wear but then my awesome daughters bought me a vest that was just a bit special (Hey Reflecto). I have added flashing lights to my helmet for night riding so I now feel very visible.
In the last year I have covered over 4000 kms on The Beast and worn out one set of brake pads. I would encourage anyone who is considering an ebike to visit your local bike shop and take one out for a proper trial ride.
Lucy Bella – Wholistic Medical Centre’s much-loved Office Manager
OUR SERVICES
OUR PRACTITIONERS
CONTACT US
1st Floor, 17 Randle Street
Surry Hills NSW 2010
Mon — Fri: 9am - 5.30pm
Saturday: 9am - 1pm