
The thyroid gland is an extremely important gland which regulates a number of complex hormonal reactions. Because of the complexity of its inter-reactions it is readily poorly diagnosed.
As an Integrative GP, I see patients on a regular basis who have been misdiagnosed or inadequately treated for thyroid problems. Thyroid function, its’ diagnosis and treatment are areas in which I have a particular interest.
The standard medical test for assessing thyroid function is to test the levels of the Thyroid Stimulating Hormone (TSH) in the blood – however this test alone is not sufficient. Patients who have apparently ‘normal’ levels of TSH can in fact have significant thyroid problems and are therefore commonly misdiagnosed.
Misdiagnosis can lead to the distressing situation where a patient is told that their thyroid function is normal when in fact it is the cause of many of their symptoms. In these cases, a patient can find themselves on the merry-go-round of being referred off to all sorts of specialists and being put on any number of drugs for symptomatic relief (eg. anti-depressants for mood disorders, statins for high cholesterol, contraceptive pill for period problems) when the real cause is right there waiting to be discovered – if only the correct tests are performed – and interpreted correctly.
Once the correct hormonal tests are performed and the genuine underlying causes determined, an effective treatment regimen can be put in place. This can give a long-lasting benefit and a whole new lease on life to people who have needlessly suffered for, sometimes, many years.
This article explains the complexities of the thyroid and its hormonal relationships in a way that is designed to be straight forward enough for a non-medical person to understand and to enable anyone to take a more proactive role in their health management.
Introduction to the Thyroid
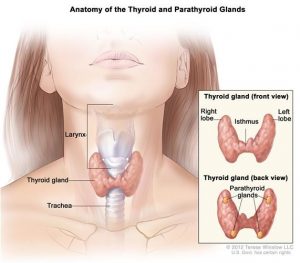
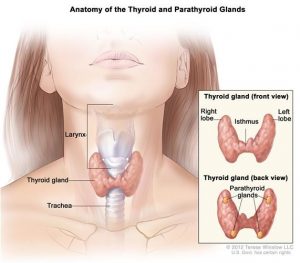
The thyroid gland is a butterfly-shaped gland in the neck, weighing less than an ounce. Its name coming from “thyros” – meaning “shield like”.
The thyroid gland is an extremely important endocrine gland in the body. It can be viewed like a ‘spark plug’ that initiates a number of vital functions, and also like a thermostat that then regulates those functions. If the ‘spark plug’ function isn’t working properly then some vital functions won’t be turned on sufficiently. If the ‘thermostat’ function is not working, then some vital functions will be either over-stimulated or under-stimulated. For effective treatment to be applied it is essential that we understand exactly how the thyroid is malfunctioning.
The vital functions that the thyroid has control over include cellular metabolism, temperature regulation, growth and development (especially foetal, and early childhood), fat breakdown, neurotransmitters in the brain and gut function.
Why talk about the thyroid gland?
Thyroid conditions are extremely common. They occur in women 10 times more often than in men and can be undiagnosed or misdiagnosed leading to years of ineffective treatment and loss of quality of life.
Of those that are diagnosed, some are not effectively managed. This can occur because the underlying causes of thyroid dysfunction are not sufficiently looked at, the interpretation of results is not sufficiently accurate or because the treatment options given may not be the best for that individual.
Symptoms
The most common symptoms of an under-functioning thyroid are fatigue, dry skin, low mood and constipation. However, because the thyroid gland controls so many functions, there can be a wide variety of symptoms. This somewhat explains how some of the misdiagnoses happen.
Other symptoms include, but are not limited to – cold hands and feet, irregular heart rate, swollen legs/ankles, puffy face, low body temperature, morning headaches, needing more sleep than usual, low heart rate, long recovery period after exercise or illness, poor immunity and recurrent infections, low libido, feeling of fullness in throat, sore throat, transient neck pain, menstrual problems, infertility, recurrent miscarriage, gut symptoms including ‘irritable bowel syndrome’ (IBS), constipation and bloating, brain fog, memory problems, goitre- neck lump, soft, weak pulse, puffiness around the eyes or face, enlarged tongue (macroglossia), voice hoarseness, slowed speech and slowed movements.
And, of course in an over-functioning thyroid, the symptoms may be the opposite. The gland may even go from under- to over-functioning.

How the thyroid gland works
It all starts in the brain and then cascades throughout the entire body! The hypothalamus gland in the brain secretes Thyrotropin-Releasing Hormone (TRH) which stimulates the pituitary gland (also in the brain) to secrete Thyroid Stimulating Hormone (TSH). TSH then stimulates the production of Thyroid Hormone T4 from the thyroid gland.
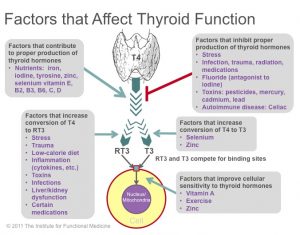
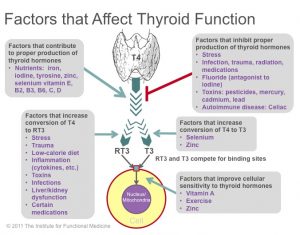
T4 itself is inactive and needs to be converted to Thyroid Hormone, T3. T3 is the main active thyroid hormone. It is T3 that does most of the work.
The conversion from T4 to T3 is done mainly outside the thyroid gland, including in the gut and the kidneys. Indeed 20% of thyroid hormones are generated via gut bacteria.
There are many factors that are needed for the conversion from T4 to T3 to happen. The main nutrients required include iodine, selenium, magnesium, zinc, iron, B vitamins (especially B2,B3,B6) and vitamin D. The main factors that can interfere with the conversion of T4 to T3 include stress, heavy metals, plastics and other endocrine disruptors, also other halogen chemicals including fluoride and chlorine.
If any part of the cascade of hormones from the brain down through the thyroid to the gut and kidneys is disrupted or incomplete, or if nutrients levels are insufficient, or if negative influences are too high – then the eventual production of T3 can be inhibited.
We can already see why simply testing for TSH can be inadequate as a diagnostic tool if the problem lies further down the chain, if the problem lies in the gut or if the problems lies in nutrition or in the presence of too many negative influencers such as stress or chemical exposure.
The pitfalls of thyroid management
TSH is the standard thyroid test that is measured.
Tests for levels of T3 and T4 are only carried out if TSH levels fall outside of ‘normal laboratory ranges’. The problem is further exacerbated by the fact that ‘normal laboratory ranges’ are generally too wide to be sufficiently sensitive to subtle variations in TSH. TSH can also be suppressed by cortisol (stress) and other illness, making it even more challenging to interpret thyroid function if we rely on TSH alone.
There is ample research showing that T3 levels are the most predictive marker of effective thyroid function – not TSH.
Even when T3 and T4 levels are tested, the interpretation of those results is very important. Again, the acceptable ‘laboratory range’ is wide and it may be that the T3 and T4 levels lie just within the ‘normal’ range but are a good way away from being optimal.
The optimal levels of T4 are 16-18pmol/L and T3 5-6pmol/L whereas the ‘laboratory ranges’ will accept readings that are significantly lower than these optimal values. This is very common and is often referred to as ‘subclinical’ hypothyroidism whereby the patient has clinical symptoms, but all the test values fall within the ‘normal’ range.
Hashimoto’s Disease
Hashimoto’s disease is an autoimmune condition of the thyroid and many patients with an underactive thyroid actually have Hashimoto’s. Diagnosing Hashimoto’s syndrome requires antibody testing which isn’t routinely done, so patients often remain undiagnosed. In still other cases, patients can be Hashimoto’s sero-negative.
The Often Overlooked role of the Gut
The critical link between the gut and the thyroid includes the following factors:
- 20% of thyroid hormones are made in the gut by bacteria
- Inflammatory gut conditions, leaky gut and autoimmune conditions of the gut are toxic to thyroid function
A good long-term solution to an underactive thyroid must therefore include a full assessment of the diet and implementation of a nutritional plan that will underpin any drug program.
But thyroxine is given for under-active thyroid – shouldn’t that fix the problem?
Thyroxine is the drug that is equivalent to T4. Sometimes taking Thyroxine is sufficient and it helps to alleviate the symptoms of an underactive thyroid.
Sometimes taking Thyroxine is not sufficient.
If there are issues with the conversion of T4 to T3 due to nutrient deficiencies, stress or toxins, then giving Thyroxine isn’t necessarily the solution. The roadblock that is preventing the conversion of T4 to T3 will also prevent the conversion of Thyroxine to T3. So, in those cases, taking thyroxine will not be very helpful. In those cases we need to investigate further and apply treatments that will genuinely work.
In some cases taking Thyroxine can actually make the situation worse!! This happens because the body can interpret high levels of emotional, chemical or nutritional stress in a way that converts T4 into a hormone called reverse T3 (RT3). RT3 actively works to shut down the thyroid gland – exactly the opposite of what is required! In these cases the more Thyroxine that a patient takes, the more RT3 that is produced and the less active the thyroid may become.
So, thyroxine has its limitations. The answer once again is appropriate testing, excellent analysis and coming to a diagnosis that pinpoints at exactly which part of the hormone cascade the problem is occurring.
Management of thyroid problems
Every person with thyroid problems is different. However, there are some common principles that apply to everyone, and then specific elements that pertain to the individual and to that individual’s specific thyroid condition.
In every case lifestyle factors need to be addressed. A healthy nutritious diet, appropriate exercise – not too little and not too much, sleep (it IS medicine!), stress management strategies, relaxation and fostering positive relationships. These are the foundations of recovery.
Supporting the adrenal and nervous system is critical. Functional and Integrative GPs like myself as well as some other practitioners at the Wholistic Medical Centre are trained in prescribing supplements and herbal medicines that can be used to help support the gut, liver, thyroid and adrenals.
Conclusion
Thinking of an underactive thyroid in simple terms, and trying to apply a single approach to what is a very complex situation will mostly lead to failure.
The good news is that when time is taken to fully understand a patient’s history, when a full suite of relevant pathology tests is run, and when a skilled analysis of all of the data is carried out, it is possible to achieve life changing results for many patients.
I hope this article provides the many thyroid sufferers with information that they can take into conversations that they are having with their medical teams.
I am very happy to respond to email enquiries and of course I am available for consultations both face to face in my rooms and also on Skype/Zoom for those that don’t live in Sydney.




















 Do you really need an MRI for your back pain?
Do you really need an MRI for your back pain?
